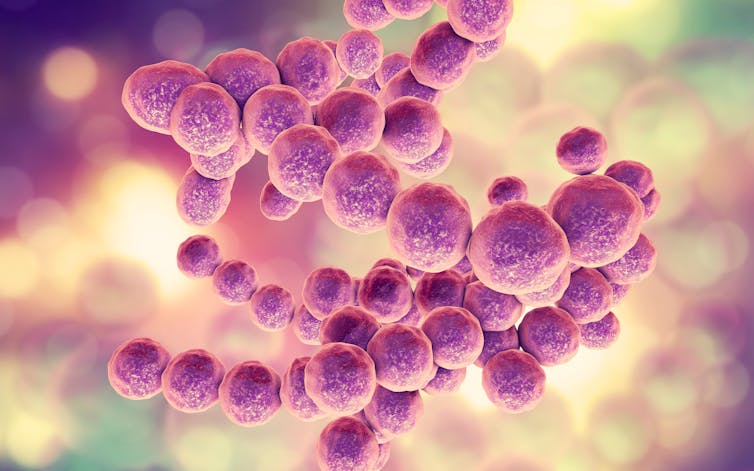
A variety of microorganisms live in our intestines, including bacteria, fungi and viruses. In summary, we refer to this as the microbiome .
Despite their tiny size, these microbes have significant impacts on our health and well-being. In fact, the microbiome is often referred to as the "second brain" due to the extensive relationship it has with the body's organs and systems.
One role that the microbes in our intestines play is supporting the Immune function . They help control local and systemic inflammation, the process by which the immune system protects us from harmful pathogens.
Therefore, it is not entirely surprising that Research has shown that the composition of bacteria in the gut can influence the severity of a COVID infection. At the same time, there is evidence that a COVID infection the balance of bacteria in the gut, which could explain why some people have persistent symptoms after a COVID infection.
The microbes in our gut provide essential signals for our immune responses throughout the body, including the lungs. A "healthy" gut microbiome includes a broad spectrum of bacteria, but is not identical in every person. Studies have already shown that a healthy gut microbiome can improve the immune response to respiratory infections by regulating immune cells and messages.
On the other hand, there is evidence that a poorer composition of intestinal bacteria increases susceptibility for influenza infections in the lungs increased and in mice to a reduced Elimination of germs from the lungs.
In COVID, too, it seems that the composition of the gut microbiome can influence the course of the disease. Research has a connection between the microbiome profile and the level of inflammatory markers in patients with COVID, where patients with a poorer combination of gut bacteria show signs of excessive inflammation. This suggests that the microbiome influences the severity of COVID infection via effects on the immune response.
Disrupting the microbiome’s balance
Just as the composition of our gut bacteria seems to affect how we fare with COVID, the opposite could also be true - a COVID infection could affect the composition of our gut bacteria. Specifically, it seems that COVID could disrupt the balance between "good" and "bad" microbes in a person's microbiome.
Studies have shown a significant difference in the gut microbiome between COVID patients and healthy people. We see a reduction in the number of bacterial diversity in the intestine – i.e. a smaller range of species, as well as considerable differences in the bacterial species present.
In particular, scientists have observed a reduction in a group of COVID patients known as commensal bacteria and act on the immune system to prevent pathogens from entering. This may increase our risk of further infections after COVID. At the same time, there appears to be an increase in a variety of opportunistic pathogenic bacteria known to cause infections.
This "imbalance" is called dysbiosis, and it has been shown that these changes in patients 30 days after infection are still present.
Recent studies suggest that intestinal dysbiosis is related to the movement of intestinal bacteria into the blood during COVID infection. In mice, COVID caused changes in a variety of parameters associated with intestinal barrier permeability, meaning that things can theoretically move more easily through the intestinal wall.
In 20% of human COVID patients in the same study, certain bacteria had migrated from the gut into the bloodstream. This group had a higher risk of developing a secondary infection in the blood.
Research now also shows that dysbiosis after COVID can lead to Long-COVID intestinal dysbiosis in patients with long-term COVID symptoms This makes sense, because dysbiosis seems to put the body in a heightened and constant Inflammatory state – something that is associated with chronic COVID symptoms.
Support your immunity
As we continue to develop a more comprehensive understanding of gut microbes and their role in inflammation, how can you help keep your immune system healthy to protect against COVID and other infections?
Certain nutrients, including Vitamins A, C, D and E as well as iron, zinc and omega-3 fatty acids all have a positive influence on the immune response against viral infections.
One Mediterranean diet , which is rich in vitamins, minerals and fiber, has an anti-inflammatory effect in the intestine. Interestingly, a bacterial strain known as Faecalibacterium prausnitzii is known, the key to immune regulation . It is often low in the Western diet, but abundant in the Mediterranean diet.
Ideally, you should avoid too much refined grains, sugar and animal fats, which all inflammations in the body.
Probiotics, supplemental mixtures of live bacteria, may also have benefits. it was shown that a mixture of bacterial strains Lactiplantibacillus plantarum and Pediococcus acidilactici reduces the amount of virus detected in the nasal passage and lungs and the duration of symptoms in COVID patients.
This combination also increased the Production of COVID-specific antibodies significant, suggesting that probiotics interact directly with the immune system and not just alter the composition of the gut microbiome.
Finally, moderate exercise also help support the immune system in fighting COVID.
, Lecturer in Genetic Immunology, Nottingham Trent University
, Professor of One Health, Nottingham Trent University
Disclosure Statement
Philippe B. Wilson is Chief Scientific Officer of NHS Willows Health.
Samuel J. White does not work for, consult for, own shares in, or receive funding from any company or organization that would benefit from this article, and has no relevant affiliations beyond his academic appointment.

